Last week, I shared my home birth story. I’m a deeply private person, a major reason for choosing to birth in my own home, so sharing the photos and graphic details about the state of my vagina in its most vulnerable moment felt like people were looking in my front window. Um, awkwaaaaaard.
I invited a very public, internet audience into my private home birth because I believe, with all my heart, that women have the right to make an informed choice about the best birthing option for themselves. It’s not weird. It wasn’t scary, risky or mysterious. And it’s not all like this mom’s scary story that’s been circulating on social media.
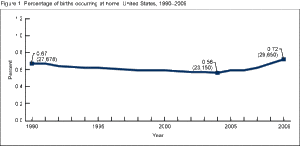 The CDC reports home births in the U.S. have increased 30% in the last few years, but still represent less than 1% of overall births. From this summary, women who are considered “low risk” and may be good candidates for home birth include a woman who is pregnant with a single baby and has made an informed choice to birth at home, baby is head down at term, spontaneous labor between 37-42 weeks pregnant, no serious medical conditions, no placenta previa at beginning of labor, no active genital herpes, no thick meconium and no prior C-section.
The CDC reports home births in the U.S. have increased 30% in the last few years, but still represent less than 1% of overall births. From this summary, women who are considered “low risk” and may be good candidates for home birth include a woman who is pregnant with a single baby and has made an informed choice to birth at home, baby is head down at term, spontaneous labor between 37-42 weeks pregnant, no serious medical conditions, no placenta previa at beginning of labor, no active genital herpes, no thick meconium and no prior C-section.
I met all of these criteria. I got my referral to Lisa, my home birth midwife of Kansas City Midwives, from my regular OBGYN’s office, although when asked for the referral letter so we could use our insurance for the birth, no one would put it in writing because of the professional stigma in the medical community for supporting home birth. A local labor and delivery nurse who doesn’t want to be identified said: “For moms who have delivered vaginally without any complications, who have also had good, routine prenatal care to rule out any complications with the baby or the pregnancy, and who is also under the care of a licensed professional doc or midwife, I see no reason why a mom shouldn’t try it if she wants.”

We’re not off the grid, we don’t buy all organic groceries, our kids attend public school, drive a minivan and work full-time. I take my kids to a pediatrician. I receive regular care from a primary care physician. I vaccinate my kids. I am a health professional myself. My husband works for a hospital system. I’m the child of a neurosurgeon and a labor and delivery, NICU nurse. I have given birth twice in a hospital, attended by an OB, with scheduled inductions and epidurals each time.When it was time for prenatal imaging (sonograms) and testing (Strep B, hemoglobin levels, etc.), I went back to my regular midwife in the OB practice so we didn’t miss any sweet in-utero pictures! If David and I had needed hospital interventions, we live within a 5-minute drive of several major hospitals.
In other words, I’m not anti-medicine. I’m not avoiding medical care. I’m using it appropriately. As a consumer of health care services, it was my responsibility to learn on my own and listen to professionals, so I could make an informed decision.
Pregnant women have a wealth of information screaming at them through emails or phone apps telling us what to pack in our hospital bags, what to expect from an epidural and suggestions for touring the hospital. During my almost 10 months of gestation, I never saw one of those apps offer me information on home birth. In a December 2014 NPR article on home birth being best for some women, our family was featured for the reasons we chose a home birth:
- It’s the safest place in the world for me, a familiar environment that allowed my body to relax and function without the physiological signs of stress from a strange environment.
- My older children were welcomed as a part of the process. Their experience has led to sensitive conversations that not enough parents are having with their children about reproduction, private parts, sex, romantic relationships, nurture, the life cycle and family.
- Home birth gave me dignity and less interventions. Did I appreciate my epidurals for my first two births? You bet your boots I did. This time though, I appreciated the respect given by my midwife. If I didn’t want a vaginal exam or monitoring of my weight (because I banished scales from my house), that was respected. My midwife danced with my changing need for distance and closeness.
The NPR article was followed by a heated commentary debate. But here’s the thing: no matter how much people debate it, home birth was right for me, my family and my newborn David. Honestly, if I planned to go to a hospital, David would have been born in the car, so it was a good thing we had a midwife come to us. A good home birth does not necessarily mean that nothing goes wrong or off-plan; but rather, when additional intervention is needed, a midwife will have a chain of resources to look after our needs. So for anyone who read my story and put on their Judgy McJudgerson hats about me “putting my baby at risk,” consider this question: what makes you feel safe?
Feeling safe is the key to a living being’s ability to carry out its natural processes. If the amygdala (an almond-shaped organ in the limbic system of the brain) sends a message to the central nervous system that says, “I’m not safe,” the body goes into fight or flight mode. The reproductive system (among other bodily systems) slows down, often stalling the birth process. Safe also applies to relationships and the environment. To me, a hospital room was unfamiliar, stark, and filled with kind nurses that were still strangers. Rather than feeling myself rise to the task of birth, I became passive and silent in the presence of institutional authority and uniforms. In my home, my body and my newborn were relaxed because I was with familiar people in a familiar place.
In January 2014, this study provided the most recent evidence of the safety of home birth. In a September 2014, the third annual Home Birth Summit brought together medical professionals, health policy regulators, ethicists, and others who believe in offering the home birth option. There are too many questions to be answered in this post by this mom, but here’s a map if you want to know more:
- Home Birth: An annotated guide to the literature (Midwives Alliance of North America)
- Outcomes of planned home births with CPMs: large perspective study in North America (British Medical Journal)
- Outcomes of planned home birth with registered midwife vs. planned hospital birth with midwife or physician (Canadian Medical Association)
- Home Birth: What are the issues? (Midwifery Today)
- Water birth (not all home birth means water birth – mine certainly didn’t).
Before I made the decision to birth at home, my midwife and I logged almost three hours in phone consultation. She later sat at our dinner table for two hours, answering more questions – an investment and attention to informed consent I’ve never had before.